Articles
Selected States’ Efforts to Educate and Address Access Challenges
In a medical emergency, do you want CPR, a feeding tube, or other life-sustaining treatment?
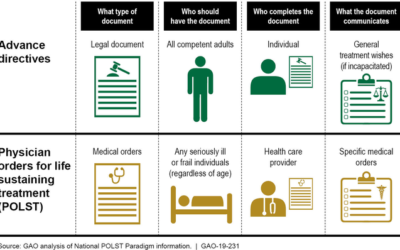
You can plan for what you want (or don’t want) using documents such as:
Advance directives—living wills and health care power of attorney—to document your health care wishes
Physician orders for life-sustaining treatment to document end-of-life treatment orders if you’re seriously ill
If you have these documents, doctors and emergency techs may not know they exist or be able to find them. And many people don’t have them.
Some states are educating health care providers and patients and maintaining document registries to address these issues.
Some advance planning documents, like this one for end-of-life care, are brightly colored to make them easier to identify.
Pre-Transplant Capture of Advanced Directives Increased from 28% to 69%
Clinicians and staff can work with patients and help them with advance care planning to ensure their wishes are respected. Californians report that loved one’s wishes are completely followed at the end of life only 44 percent of the time (1).
City of Hope is addressing the gap by making it easier for clinicians to document and view patients’ decisions as part of a comprehensive advance care planning initiative. As part of their Plan Today for Tomorrow initiative, City of Hope focused on the hematopoitetic stem cell transplantation (HSCT) population and incorporated obtaining advance directives into their new patient orientation and pre-transplant education classes. They also implemented a co-rounding model between palliative care and medical oncology for late-stage cancer patients and designed a standard process for verifying advance care planning documents.
To supplement their care model, City of Hope introduced Epic tools to:
Prompt clinicians to discuss code status with patients.
Help clinicians document more detailed treatment preferences and use the appropriate billing codes.
Clearly show when comfort care for actively dying patients is initiated.
In just two years, City of Hope saw the advance directive completion rate for HSCT patients increase from 28.6 percent to 69.5 percent (2). As your organization develops a care model for advance care planning, you can use Epic tools similar to City of Hope to support your program and help ensure that patients’ wishes are known and respected throughout the continuum of care, especially in their last days.
This program was designed and implemented by Finly Zachariah, M.D., Assistant Clinical Professor of Palliative Medicine and Supportive Medicine, and his team at City of Hope.
Telehealth Platform for Amazon Alexa
“We have a bold vision of the future: All care that can be digital will be digital, and all care that can be done in the home or in the community will be done in the home or in the community,” Janice Nevin, MD, MPH, CEO of the three-hospital health system, said in a press release. “Engaging patients digitally is more important than ever right now, as it will help them reach their health goals, improve their experience, and shape the future of health care as we know it.”
“Voice assistants are in millions of homes in the US,” Randy Gaboriault, ChristianaCare’s chief digital and information officer, said in the press release. “By leveraging this technology, we are creating a new model of care within patients’ homes to support the best health outcomes possible.”
KPMG ‘Bots in rev cycle
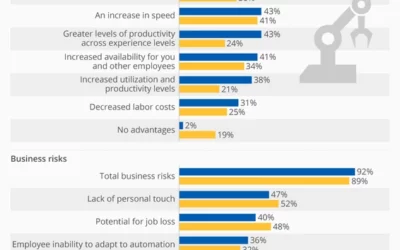
Hospitals are in a bind. As the shift toward value-based contracts intensifies, revenue cycle operations are becoming increasingly complex. Payers are exploring new ways to quantify value as it relates to reimbursement, which puts additional pressure on hospitals to provide documentation to support claims. Even positive developments such as lower unemployment have led to higher labor costs. All of this has the potential to decrease hospitals’ cash flow and negatively impact the bottom line. Hospitals increase revenue recovery with robotic process automation AI is defined as the combination of cognitive automation, machine learning, reasoning, hypothesis generation and analysis, natural language processing, and intentional algorithm mutation to produce insights and analytics at or above human capability.
Robotic Process Automation in the Healthcare Industry
COVID-19 has had a massive impact on healthcare providers. Dire need has pushed many healthcare professionals to the limit to the point of affecting their own health.
According to Gartner, 50% of US healthcare providers will invest in RPA over the next three years. Artificial Intelligence (AI) enablement within clinical or nonclinical processes for patient interactions, which is a mere 4% today, will increase at least five fold.
Overview of Robotic Process Automation in the Healthcare Industry
According to a report published by the United States Census Bureau in 2016, a new demographic trend has emerged. By 2020, people over the age of 65 will outnumber children under 5. And by 2050, the percentage of people 65 and over will be more than twice the percentage of young children. This so-called “demographic earthquake” is expected to start taking effect on the global labour market.
This means, among others, that the number of people who need medical assistance is also on the rise. The healthcare industry must find the resources to adapt to this new demographic trend. Robotic process automation in healthcare should thus be taken full advantage of, in the attempt to provide adequate medical care to a larger number of people.